|
Rotation Policies & Procedures
Wards
Last Updated: 06/2019
I. Guidelines and Policies General Policies
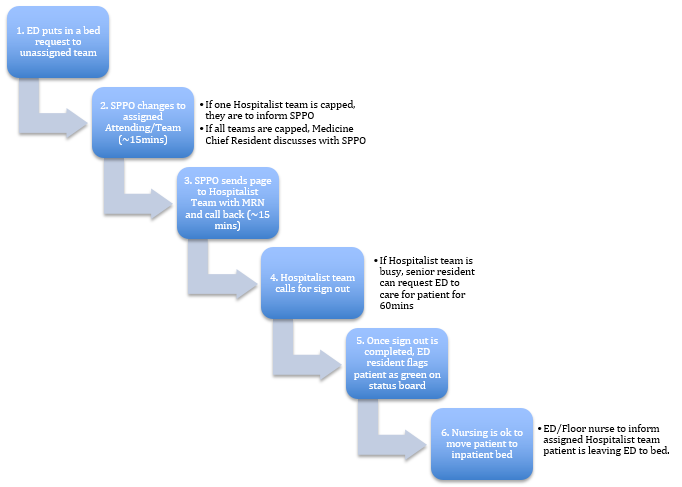
A. Admission Workflow
- ED Admissions
- ED resident/attending will place bed request to unassigned team once decision has been made to admit patient to hospital
- SPPO will update order with assigned team and attending based on which team is next up and send page to team admission pager.
- All admitting teams (including short and long call teams) will be assigned patients per drip beginning at 6:30AM. Short call teams will admit to 5:00PM, while long call teams will admit until 7:00PM.
- Any teams that are capped will not be in drip for admission. Medicine resident is responsible for notifying SPPO if they are capped
- If all teams are capped, SPPO will contact Medicine Chief Resident to discuss team assignment (see Overflow Admissions below)
- Once notified, Medicine resident will contact ED resident/attending for signout within approximately 15 min.
- If team is not able to immediately assume care of patient, Medicine resident will contact ED resident/attending to acknowledge and request ED continue to manage patient for 60 minutes. Within this time, Medicine resident will call back to receive full signout and assume care.
- Once signout is complete, ED resident will flag patient as "green" on status board. Once status is changed, nursing may move patient to inpatient bed.
- Outside Hospital Transfers
- All accepted patients will be added to patient log on SharePoint by accepting hospitalist.
- SPPO will assign incoming outside hospital transfers to admitting Medicine teams and notify respective team
- Medicine resident will place admission orders prior to or at time of patient arrival
- In event patient is assigned to team but does not arrive prior to signout, accepting team will place initial admission orders and start initial H&P note. Admission will be completed by crosscover night float resident once patient arrives.
- See E. Outside Hospital Transfers below for additional details
- Overflow Admissions
- In event multiple or all teams are at ACGME hard cap, SPPO will contact Medicine Chief Resident to discuss assignment for patients pending admission.
- Depending on status of other admitting teams and following discussion with program director, one or more of the following contigency plans below may be initiated:
- Backup Resident: Resident will admit and crosscover new patients until teams are able to assume care
- Team H Residents: Residents will admit and crosscover new patients; they may either sign patients out to ward teams, or serve as primary service depending on patient needs, team censuses per discussion with Chief Resident.
- Family Medicine service: Family Medicine residents will admit directly to inpatient FM service per Overflow Policy (see "Overflow Policy" under Family Medicine below)
- Nurse Practitioner: Inpatient nurse practitioners will admit patients, which will be managed under supervision of non-call attending(s)
B. Caps
- Team cap is defined as:
- 20 patients per team
- Note: Soft cap eliminated as of 01/2019
- Daytime Admissions
- Any team that reaches the cap will be out of the drip until their census drops below 20 patients
- Teams must notify SPPO office (x8455, p6000) they are capped.
- Teams must notify SPPO office when they are uncapped and able to re-enter drip. Patients who have received all discharge instructions and are waiting for rides (either on the floor or in the discharge lounge) do not count towards the total team census
- Overnight Admissions
- Teams that will be are at cap will be out of drip for all overnight admissions.
- Overflow Admissions
- In event all admitting teams are at cap, admissions will be assigned per Overflow policy (see Admission Workflow above)
C. Bouncebacks
- Bouncebacks follow the senior resident for the current block except in the following situations
- Team is no-call and senior resident is not present
- Team is at or above soft cap and other teams are open
- It is the first or last day of the block
- If patient cannot bounceback to original team due to one of above reasons, they should be assigned to next admitting team.
- Patient will be transferred back to original team the next day. Original team does not receive credit for admission, as staffing and workup/management will already have been initiated at this point
- During day time, if admitting team receives a patient found to be a bounceback to anothre team, senior resident should notify SPPO immediately for patient to be reassigned to appropriate team.
- Patients primarily being managed by NP who bounceback should be admitted to original team unless they are at or above soft cap. If team is open, they may take bounceback regardless of call status or presence of senior resident. These patients will be managed by NP and attending.
D. MICU/CCU Transfers
- Patients transferred from the MICU or CCU to wards will be assigned to an admitting ward teams by SPPO office. MICU/CCU resident will be responsible for notifying SPPO if patient is bounceback to a team, Family Medicine etc. and can take patient based on Bounceback rules (see above).
- Daytime Transfers (6:30AM-5:00PM)
- Admitting team will receive signout from MICU/CCU intern/resident. Once signed out, admitting team has primary responsibility for patient care
- If there is a patient emergency while patient is still in ICU, MICU/CCU team should assist, if possible, and notify admitting team immediately
- Admitting team will evaluate patient and write an accept note in EPIC
- Admitting team will sign out patient to night float regardless of where patient is physically located
- Management of patient over night (i.e. by Ward vs. MICU night float) will be determined by patient's physical location at 5:00PM
- Wards crosscover resident will manage patient if on the floor
- MICU resident will manage patient if still in ICU. Admitting team will resume care in AM.
- Long Call Transfers (5:00-7:30PM)
- Admitting team will be assigned MICU/CCU transfer by crosscover night float resident
- Admitting team will receive signout from MICU/CCU, evaluate patient and write an accept note.
- All patients transferred during long-call will be managed by MICU night float resident, even if patient is physically moved to wards during evening or overnight
- Both admitting ward team and MICU team should sign out patient to respective night float teams
- Overnight Transfers (7:30PM-6:30AM)
- SPPO will notify admitting residents (via pager) of any MICU/CCU patients with pending transfer orders who are transferred to floor overnight
- Admitting night float residents will log these patients and notify day teams of transfers at AM signout
- Admitting day teams will be responsible for contacting MICU/CCU team in AM to receive signout and assume care
E. Outside Hospital Transfers
- All outside hospital transfers are accepted by the hospitalist attending on-call
- Patients may be accepted as transfers for higher level of care, continuity, insurance issues etc.
- On accepting patient, hospitalist will enter patient into SharePoint site, with basic details and guidance on case
- SharePoint may be accessed via residency website, intranet, or by using this link: https://intranet.ha.uci.edu/sites/deptofmedicine/res/intmed/default.aspx
- UCI Transfer Center (x2222) may be able to provide additional details, including outside hospital records, if patient being transferred from inpatient unit. Patients being transferred from outside ER may not have records available
- Outside hospital transfers will be assigned to team by SPPO at time of acceptance. However, patient may not arrive until later in day or overnight
- In event outside transfer does not arrive by time of signout, admitting team is responsible for entering basic admission orders and starting a skeleton H&P based on available info.
- Patient should be signed out to night float crosscover resident, who will complete admission (with physical exam, additional orders etc) when patient arrives.
F. CDDC/GI Admissions
- Patients may require transfer from CDDC to inpatient wards under the following circumstances. Decision to admit to hospital (vs. monitor in CDDC observation unit) is at the discretion of the GI attending
- If GI fellow/attending feel patient will require extended (>47hr) observation or higher level care immediately post-procedure
- If patient was initially admitted to CDDC observation unit but has or will require observation or care beyond 47hrs
- GI patients to be admitted to ward will be assigned to admitting teams by SPPO
- Admitting team will assume care of patient once they have been physically transferred to inpatient unit, e.g. PPCU, floor, ICU, etc.
-
- If patient has any issues while in CDDC, these should be taken care of by CDDC daytime hospitalist or GI fellow/attending
- If patient is not physically transferred to inpatient until by 5:00PM, admitting team should enter basic admission orders and start skeleton H&P (see Outside Hospital Transfers above)
- Residents, including MICU team, are not responsible for evaluating patients for admission. As noted above, decision to admit is at the discretion of the GI attending.
G. Team O
- Census
- Team H residents
- If total Resident census is less than 8, they can take Team O admissions up to total census of 8 and would continue to follow those primary patients
- If their census is 8 or more, they only take Team H consults up to the Resident cap
- Team O NP
- Team O NP will have a cap of 8
- Admissions then go to Team H resident if their census is less than 8, otherwise Team O Attending needs to call Chief Resident to cap Team O.
- If Team O census is less than 8, CDDC patients count towards cap but if Team O census is more than 8, then CDDC patients still go to Team O but ED patients do not
- All Team O patients (including Team O patients on Team H) are to be signed out to the overnight NP
- Process to Cap Team O
- Team O Attending can make the decision to cap Team O. Once this decision is made, the Team O Attending will inform the on-call Chief Resident who will notify SPPO
- Team O Attending will notify on-call Chief Resident when Team O is available for resuming admissions
- Admissions
- Team O Admissions
- ED Physician to work with ED Case Manager to determine if a patient should be admitted to Team O
- ED Physician enters a direct admit from clinical order as ‘medicine unassigned’
- SPPO will notify Team O
- NP will contact Team O Attending immediately with admission notification, and the Team O Attending will respond to ED immediately and make a decision on admission vs observation vs discharge within 30 minutes
- Changing Admission Class in ED
- Team O NP/Attending can change admission class from Observation to IP after discussion with ED Case Manager to understand necessary criteria to meet IP status and then notify SPPO/Ward team of admission without further involving ED.
- THE QUESTION TO ASK THE ED CM IS WHAT CRITERIA WOULD QUALIFY FOR AN INPATIENT STATUS. IF THAT CRITERIA IS EXPECTED TO HAPPEN DURING THE INPATIENT STAY THEN THE PATIENT CAN BE CONVERTED TO INPATIENT STATUS. If no CM is present, then Team O NP/Attending can reach mutual agreement with ED Attending and Team O will notify SPPO/Ward Team. Team O Attending to communicate necessary IP criteria with ward attending
- Patients converting from Observation to IP
- Once already admitted to Team O/H, any patients that need conversion from Observation to IP status will remain on Team O/H until discharge
- Bounce Backs
- Bounce back patients are to return to the original team that they were discharged from
- Attending
- Team H attending will serve as primary attending for Team O during the day
- Nocturnist (attending assigned to Team O/CDDC) will serve as primary attending for Team O over night
Service Agreements & Policies
Criteria are summarized below for each respective service. For additional details, please see full service agreement (located under "Policies" on residency website)
A. Family Medicine
Last Updated: 01/24/2020
- Admission Criteria
- In order to be admitted to Family Medicine service, patients must be ALL of the following criteria
- Patient identifies a UCI Family Medicine or Geriatrics provider as their primary provider, and intends to follow up on discharge from hospital
- Patient has been seen for at least 2 visits during the previous 2 years by 1) any Family Medicine resident, 2) Family Medicine provider, or 3) Geriatrics provider at their outpatient clinic site (FQHC Santa Ana, FQHC Anaheim, Gottschalk Medical Plaza, UCI Senior Center, PACE clinc (if attending is FM faculty)
- These two visits are to be continuity visits (not just urgent urgent care)
- To avoid disruption in continuity of care, patients should not be transferred between services after day team has acquired the patient.
- Family Medicine/Geriatrics providers include:
| Arghami, Elham MD |
Arroyo, Jeff MD |
Austin Rachel |
Biddy, Edna MD |
| Centanni, Leah |
Craemer, Elana MD |
Deshpande, Prajakta MD |
Doloulei, Reza MD |
| Dow, Emily MD |
Gibbs, Lisa MD |
Haq, Cynthia MD |
Khalighi, Katayoun MD |
| Kilgore, David MD |
Kim, Brian MD |
Kroner, Christopher MD |
Larsen, Kathyrn MD |
| Mayorga, Jose MD |
Morohashi, David MD |
Nguyen, Tan MD |
Prislin, Michael MD |
| Raymundo, Marianita MD |
Salcedo, Betzy MD |
Seghal, Sonia MD |
Suskin, Shea MD |
| Tam, Steven MD |
Tran, Huy DO |
Vadecha, Nina MD |
Valerie George, PA-C |
| Vega, Charles MD |
Vo, Baotran, MD |
Whalen, Megan |
|
- Caps
- Capped at 15 patient (including pediatrics and OB)
- Once the cap above is hit for the FM service, the next patient with a senior health center PCP will go to Internal Medicine service and the next patient with a PCP at the FQHC will go to Family Medicine service.
- Once FM hits 15 adult patients, then all patients will go to the IM teams until the FM team uncaps. If all teams are capped above 15 then everyone will share the overflow and continue to take admissions.
- Overflow Policy
- In event all IM admitting teams are at or above 18 patients, FM will assist with admissions as below:
- If FM uncapped: Service will get inserted into drip and take both Medicine and FM patients
- If FM and IM capped:
- FM will admit all FQHC-Santa Ana/Anaheim patients
- IM will admit all Senior Health Center patients
- Patients may be distributed across any team at the discretion of the Hospitalist Executive Director, Dr. Amin.
B. Cardiology
Last Updated: 11/15/2018
- Admission Criteria
- Cardiology Service (CCU or Telemetry)
- Newly identified acute heart failure decompensation without other acute noncardiac medical problems
- NYHA class III-IV heart failure considered having high in-hospital mortality (BUN>43, SBP<115, and serum Cr>2.75 (excluding patients with CRF or on hemodialysis))
- Suspected or diagnosed acute coronary syndrome (unstable angina, acute myocardial infarction, aborted sudden cardiac death)
- Newly identified and/or potential life-threatening symptomatic arrhythmia (sustained ventricular tachycardia, high-grade atrioventricular block, symptomatic atrial fibrillation, persistent symptomatic brady- or tachyarrhythmia
- Acute decompensated heart failure requiring or at risk of requiring invasive ventilatory support
- Cardiogenic shock or otherwise requiring chemical or mechanical circulatory support (dopamine, dobutamine, milrinone or adrenergic agonist drip, IABP counterpulsation, LVAD)
- Patient regularly followed by member of Cardiology department and without other acute noncardiac medical problem.
- "Regularly followed" defined as two clinic visits within last 12 months
- "Without other acute noncardiac medical problem" defined by best clinical judgment and decision of ED attending
- Medical ICU Service
- Multisystem organ failure
- Requiring or at risk of requiring invasive ventilatory support, excluding acute decompensated heart failure
- Hospital Medicine
- Acute decompensated heart failure not meeting any of above admission criteria, with Cardiology Nurse Practitioner consult
- Following patients, with consideration for urgent Cardiology consultation:
- Persistent or worsening symptoms despite aggressive and sustained intervention.
- Diastolic dysfunction of unclear etiology.
- Inodilator or vasodilator infusion with worsening of heart failure.
- Suspected acute coronary syndrome (i.e. unstable angina, acute myocardial infarction, aborted sudden cardiac death, unexplained abnormal cardiac enzymes).
- Suspected significant coronary artery disease who are candidates for diagnostic angiography/percutancous or surgical coronary intervention.
- Abnormal provocative stress-test who are candidates for diagnostic angiography/percutaneous or surgical coronary intervention.
- Undergoing evaluation for or post cardiac transplant
- Newly identified serious arrhythmias (e.g. ventricular tachycardia, symptomatic brady or tachyarrhythmias, high grade a-v block).
- Destabilized chronic/known arrhythmias.
- Implanted mechanical devices (e.g. LVADs).
- Implanted electrical devices that require interrogation or are suspected of malfunction (e.g. pacemaker, AICD)
- Candidates for cardiac resynchronization (i.e persistent symptoms + EF <35% + QRS interval > .12 sec).
- Currently regularly followed by a member of the Cardiology department (as defined above)
- For evaluation for transfer to Cardiology service
- Readmission/Bouncebacks
- Heart failure patients readmitted within 30 days should be readmitted under the previous team unless condition requires different admission services as best decided by clinical judgment of ED attending
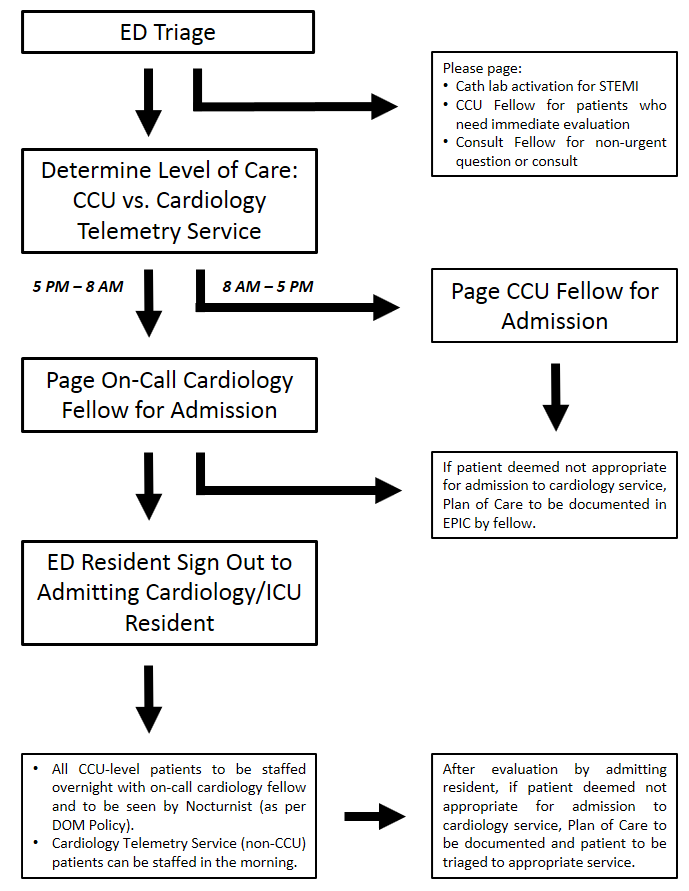
- Admission Workflow
- ED resident will evaluate patient for possible admission to Cardiology service (including both telemetry and CCU level of care) based on Cardiology admission criteria (see below).
- ED resident will contact appropriate Cardiology fellow for acceptance to Cardiology service. Medicine residents cannot accept patients to Cardiology service, and should not be contacted prior to approval from fellow
- 8AM-5PM: CCU Fellow
- 5PM-8AM: On-Call Cardiology Fellow
- Once Cardiology fellow has accepted patient to Cardiology service, ED resident will contact admitting Medicine resident for signout.
- Any patients deemed not appropriate for admission to Cardiology service by fellow will require Plan of Care documentation in EPIC, with further recommendations, if appropriate.
- For daytime admissions:
- Patients will be staffed with daytime Cardiology service attending per usual schedule
- For overnight admissions:
- Admitting Medicine resident will contact on-call Cardiology fellow to staff all CCU level admissions
- Non-CCU (telemetry) level patients may be staffed by primary team in the morning. However, residents are encouraged to contact on-call Cardiology fellow with any questions that arise.
- Nocturnist will also see all CCU level patients per Department of Medicine policies
C. Hematology/Oncology
Last Updated: 03/28/2017 Team L Policies
- Admission Criteria and Policies
- Patients with established diagnosis of hematologic malignancies (categories listed below) on active treatment for their neoplasm:
- Any Acute Leukemia, Myelogenous or Lymphoblastic (AML or ALL respectively
- Chronic Myelogenous Leukemia
- Chronic Lymphoid Leukemia
- Lymphoma (Hodgkins or Non-Hodgkins)
- Multiple Myeloma
- Myeloproliferative Neoplasms (for example P. Vera)
- Myelodysplastic Syndromes (for example, myelofibrosis)
- Patients with established diagnosis of hematologic malignancies but admitted for reasons other than receiving anti-neoplastic therapy will be admitted to the Hospitalists service(s) and followed by the consult service (Team S, see below).
- Team L will have a cap of 16 patients until further notice
- Direct admissions, admissions through the ED, and transfers from other services require the notification of and approval of the Team L attending.
- No patient will be transferred to Team L without the express consent and agreement of the Team L attending.
- Neuro-Oncology Primary CNS lymphoma patients will be on Team L only if receiving active anti-lymphoma treatment. Other neurologic oncology patients and neuro-oncology primary CNS lymphoma patients not receiving treatment will be on admitted to Neurology.
- Admissions occurring (arriving on the floor) between 7:00 AM and 5:00 PM will be admitted by one of the advanced practitioners (APs) on Team L.
- Admissions occurring outside of the above time period will be admitted by the MICU and/or night float resident with an appropriate note and orders, with the management plan developed in conjunction with the Team L attending on call. All patients must be staffed with Team L attending.
- Cross Coverage
- The Team L patients will be signed out to MICU and night float by one of the AP staff or Team L fellow on behalf of the entire team, with similar sign out to the faculty attending at 6:00 PM.
- Patients on Team L needing acute management will be covered after 6:00 PM until 7:00 AM by the night float and MICU teams until further notice. It is expected that the Attending and/or Heme/Onc Fellow will be actively available throughout this time to answer questions, facilitate in diagnosis and management, and come in to evaluate patients if needed.
- The nursing staff will be instructed to contact the NP/AP or Fellow during regular business hours M-F (0700 to 1800) for questions regarding the respective assigned patients.
- The nursing staff will be instructed to page the night float/MICU team for emergency situations requiring immediate physician evaluation and intervention, outside of regular business hours (0700 to 1800.
- The nursing staff will be instructed to page/contact the Team L Faculty Attending for routine questions/concerns/orders/responses to laboratory determinations, etc. from 1800 to 0700, 7 days a week.
- During weekend days, regular business hours (0700 to 1800), a clinical fellow will be available “on call” for Team L until such time as the full compliment of APs are in place.
- Daily Workflow
- Team L will have “working rounds” that, 1) start at 8:30 AM, 2) include the nurse assigned to each patient, and 3) incorporate multidisciplinary discharge rounds between 10:30 and 11:00.
- The Team L attending will be responsible for the distribution of patient assignments, to be distributed equitably between members of the team (advanced practitioner, faculty attending, and/or clinical Fellow).
- All clinics will be blocked for Team L Attending faculty, as the Attending is required to be physically available to the advanced practitioners during regular business hours M-F (0700 to 1800).
Team S Policies
- Admission Criteria
- All patients with documented malignancies that are non-hematologic in origin will be assigned to one of the Internal Medicine (Hospitalist) teams or other non-Team L services.
- Patients with a presumptive diagnosis of neoplasm, hematologic or nonhematologic, will be assigned to one of the Internal Medicine (Hospitalist) teams or other non-Team L services.
- Team S will function as a consult service for these patients.
- If and when a diagnosis is established for a hematologic malignancy, the patient can then be transferred to Team L, with Team L attending approval.
- Hematology/Oncology patients presenting to the ED and requiring admission will be triaged through the Team S fellow for possible admission to Team L (see above) or to another inpatient service.
- Inpatient Chemotherapy
- Chemotherapy for patients with non-hematologic malignancies, if needed as an inpatient, will be overseen by the Team S fellow and attending being comanaged with the primary attending service (guidelines below):
- a. Team S will be responsible for writing and submitting the orders for and the coordination of the administration of chemotherapy.
- b. This includes, all premedications, anti-emetics, IV fluids, and post chemotherapy growth factors if needed
- c. Team S will document the specifics and details of the chemotherapy regimen, inclusive of issues (toxicities or complications) to be aware of within the body of their consult progress note.
- d. Team S will meet with the Medicine team and provide chemotherapy education, specific to the chemotherapy regimen and general principles of management of patients receiving chemotherapy.
- e. Team S will provide a schedule for laboratory and radiographic monitoring and will be available for questions from the primary team.
- The administration of chemotherapy will require coordination with chemotherapy certified nursing staff (likely from 76/78) and/or relocation of the patient to 76/78, depending upon bed and staffing availability.
- Daily Workflow
- The usual PBG and Medical Staff requirements for timely consults and professional, timely communication will be enforced.
- Team S faculty will have either their AM or PM clinics blocked to facilitate timely and productive interactions with the admitting teams.
- It is the expectation that in-person communication and education will occur with the team during or juxtaposed to the Hospitalist Team rounds.
- Patients with established diagnosis of hematologic malignancies who are admitted to other services besides Team L may be staffed by the Team L attending in conjunction with the Team S fellow.
- Team L and Team S attendings are expected to coordinate their “rounds” with the Team S consult fellow.
- The Team S fellow, or similarly assigned “on call” clinical fellow, will remain “on call” for outpatient calls through the call center, after hours, regardless of patient diagnosis.
- It is the expectation that the Team S fellow will maintain communication with individual patient’s outpatient faculty attending throughout the course of their hospitalization.
D. Orthopedics
Last Updated: 03/01/2013
- Admission Criteria (applies only to elderly patients with fractures)
- Trauma Surgery
- >=60years with multiple trauma, including orthopedic injuries, with Orthopedics consult
- Medicine Consult service (Team H) may be consulted, as necessary, for management of medical issues
- Hospital Medicine
- >=60yrs with fractures without other traumatic injuries, with Orthopedics consult
- Admission Workflow
- Orthopedics will evaluate patients in ED and perform appropriate evaluation and splinting
- For operative candidates, Medicine (either primary hospitalist service or Team H) will perfrom appropriate medical workup and medically optimize patient, as appropriate.
- Patients admitted to Hospitalist service overnight will undergo preoperative evaluation by night float resident. Night float resident will staff preoperative recommendations with ICU nocturnist
- Once optimized, Orthopedics will perform surgery within 24 hours
- Orthopedics will be responsible for arranging followup for all patients. Follow up appointments, wound care and activity restrictions should be noted in discharge instructions and summary by Orthopedics team.
E. Courtesy Notifications
The following services should be notified if their established patients are admitted to the inpatient ward services:
- Hematology/Oncology
- Notify primary oncologist of any patient admitted to ward service
- If patient requires inpatient Oncology consult, notify the Hematology/Oncology consultservice (Team S)
- All goals of acare discussions regarding established patients need to be discussed between fellows and/or attending physicians, and should not be initiated by residents
- Nephrology
- Notify Nephrology fellow or attending for all patients on active hemodialysis who are transitioned to comfort care.
- Transplant Nephrology
- Notify Transplant Nephrology fellow or attending for all patients with history of renal transplant admitted to hospital
- Transplant Surgery
- Notify Transplant Surgery resident or attending for all patients with history of organ transplant admitted to hospital
- Cardiology
- Consult Heart Failure Nurse Practitioner for all patients admitted to the hospital with acute decompensated heart failure.
- Primary Care
- PCPs for all patients with established care at UCI (including Pavilion III, Gottschalk Plaza, and Senior Health Center) should be notified of admission and discharge
- On discharge, an encrypted email with brief description of hospital course and important follow-up information should be sent
II. Rotation Logistics
Schedules
A. Daily Schedule
| 6:30AM |
AM Signout (Team C Workroom) |
| 7:00-8:00AM |
Prerounds |
| 8:00-9:00AM |
Morning Report (Tu/Th/Fri) |
| 9:15-9:30AM |
Interdisciplinary Rounds |
| 9:30-12:00PM |
Attending Rounds |
| 12:00-1:00PM |
Noon Conference |
| 1:00-5:00PM |
New admits, discharges |
| 5:00PM |
PM Signout (No, Short Call teams)
Long Call teams admit up to 3 patients between 5:00-7:30PM* |
| 7:30PM |
PM Signout (Long Call teams) |
*If team is soft-capped (at 18 patients) at 5:00PM, they will continue to admit until 6:30PM, and may take up to 3 admissions or until their census reaches 20. (See Call Schedules below)
*If long call teams receive all admissions (up to 3 per team), admitting night float residents will come in at 6:30PM to start admitting. Cross-cover resident will be responsible for notifying admitting residents if they need to come in early.
B. Call SchedulesFour ward teams will be on-call to admit new patients on any given day. Teams will admit patients according to a modified drip system, with all patients (including admissions from ED, outside transfers, direct admissions from clinics) assigned by SPPO.
Call Structure
- No Call Teams
- Teams will not accept any NEW patients during day unless approved by attending
- Team may accept bouncebacks cared for by intern/resident on no-call day if senior resident is present.
- Team may accept bouncebacks cared for by nurse practitioner regardless of whether senior resident is present or not. These patients will be managed by NP and attending.
- Short Call Teams
- Teams will accept new patients per drip system up to 5:00PM
- Long Call Teams
- Teams will accept new patients per drip system up to 7:30PM
- Teams that enter long call at soft-cap (18 pts) will admit up to 2 patients until 6:30pm.Any additional admissions beyond 6:30PM will be admitted by night float admitting residents.
- Teams that enter long call below soft cap will admit up to 3 patients until 7:30pm.
Admission Caps
- Team Cap: 18 patients (soft-cap), 20 patients (ACGME hard-cap)
- Teams cannot be actively responsible for more than 20 patients at any time
- Intern Cap: 10 patients, 8 new H&Ps in 24 hour period (does NOT include overnight admissions)
- Senior Cap: 20 patients, 10 new H&Ps, plus up to additional 4 transfers in 24 hour period (does NOT include overnight admissions)
Educational conferences are held throughout the week (no conferences on weekends or holidays).
Attendance at morning reports (Tue, Thu, Fri AM) is required for all residents at UCI, including those on inpatient and elective rotations, and those on Y-week (unless conflicting with your scheduled clinics).
Attendance at Academy of Medicine conference is required for all residents on elective rotations and Y-week.
|
MON |
TUE |
WED |
THU |
FRI |
| AM |
|
AM Report
8:00-9:00AM (DH 78)
Case Conference |
|
AM Report
8:00-9:00AM (DH 78)
Case Conference |
AM Report
8:00-9:00AM (DH 78)
Night Float Report
Academy of Medicine
9:00-12:00PM (DH 78)
|
| PM |
Noon Conference
12-1PM (Bldg 22) |
Noon Conference
12-1PM (Bldg 22) |
Noon Conference
12-1PM (Bldg 22) |
Noon Conference
12-1PM (Bldg 22) |
Noon Conference
12-1PM (Bldg 22)
|
D. Day Off Policy
Senior Residents
- Will take three days off over course of block (averaged to one day off per week)
- May only take no-call days off. Senior residents cannot be off on any day team is admitting
- May not take same day off as MS-4 subinterns (if present)
Interns
- Will take three days off over course of block (averaged to one day per week). Prelims residents on for >3 weeks will take one day off per week worked.
- Days off are assigned at the discretion of the senior resident and attending.
- Should not take long-call days off unless permitted by senior resident and attending
- Days off should be scheduled at beginning of rotation to ensure appropriate coverage for block
Medical Students
- MS4: Will follow same days off rules as interns
- MS3: Will take one day off per week. May only take Saturday or Sunday off, unless permitted to do otherwise by clerkship. (See Medical Student Policies below)
Ward Logistics
A. Handoffs
AM Signout
- Occurs at 6:30AM each morning. All team members, including senior resident are expected to be physically present to receive signout
- Location of signout (i.e. all signout in Team C workroom, vs. cross-cover signout in Team C, admissions signout in Team G) at the discretion of the night float team
- Senior resident is responsible for assigning new patients and providing cross-cover information to interns, sub-I's and NPs.
PM Signout
- Occurs at 5:00PM for No Call and Short Call teams, and 7:30PM for Long Call Team
- All PM signout will take place in Team C workroom. It is up to the discretion of the team who is present for signout.
- Signout for NP patients
- If senior resident is present: NP is expected to sign out their patients to senior resident no earlier than 4:45PM. Senior resident will be responsible for signing these patients out to cross-cover resident
- If senior resident is off: NP is expected to sign out their patients directly to crosscover resident at 5:00PM. Interns should NOT be involved in cross-coverage of NP patients
- Use the "General Medicine" (not "Hospital Medicine") handoff template in EPIC
- Use the I-PASS technique and ensure that written handoffs are complete, pertinent and updated
B. Code Blue/RRTs
The Code Blue/RRT pager will be staffed by the following residents/teams:
- Day (6:00AM-6:00PM): MICU senior resident, Team H resident
- Night (6:00PM-6:00AM): MICU night float resident, Wards night float cross-cover resident
C. Notes/Documentation
The following policies are in place regarding required documentation on wards:
- All patients need one note per day that the attending sees the patient. If a patient is admitted later in the day or overnight and staffed the following day, the H&P is sufficient and an additional note is not required
- However, if there are significant changes or deviations from the initial H&P, an updated event or progress note should be written
- No progress note is required on day of discharge. The discharge note can be used as the note for the day.
- Patients who are transferred to the wards service from MICU or CCU in the afternoon or overnight do not require an additional progress note on the day of transfer (as MICU/CCU progress signed by critical care attending is sufficient.) A progress note is required for the following day, when the patient is staffed with the ward attending.
- Medical student notes CANNOT be used in lieu of required daily progress note. This includes notes that are initiated or primarily composed by medical students, even if they are revised by a resident.
D. Duty Hours
All residents are responsible for logging duty hours in New Innovations. Duty hours should be accurately recorded according to hours worked.
Per ACGME guidelines, all residents (interns and senior residents):
- May work a maximum of 24 hour shifts, plus 4 hours for transitions of care
- Must have at least 8 hours off in between shifts
If an intern or resident feels they are in danger of violating work hour restrictions, they should contact the chief resident as soon as possible to discuss scheduling.
E. Medical Student Policies
Orientation
- All MS3s will complete orientation on rotation with clerkship director and chief residents prior to first day of work
- Alls MS4 sub-interns will receive orientation from clerkship director prior to first day of work.
- Any questions regarding clerkship policies, grading, requirements, etc. should be directed to clerkship coordinator or director
Schedule/Duty Hours
- MS3s will follow their team's call schedule Mondays to Fridays. Medical students should be excused at time of signout (5:00PM or 7:00PM)
- All MS3s will have their scheduled day off on Saturdays for weeks 1-3. They will have both Saturday and Sunday off ("golden weekend") on week 4 of their rotation.
- MS3s will follow the schedule below on Sundays, depending on their team's call:
- Students on the short or long call days will report to their regular assigned teams for admissions starting at 12 PM.
- They are excused from rounds prior to 12 PM. If they arrive at 12 and attending rounds are still occurring, then they are expected to participate on rounds.
- If a patient is admitted at any time during the students’ shift, the student should admit the patient.
- Students are expected to stay for the duration of the call shift.
- Sunday night shift schedule (night shift teams):
- Students on the night shift days will report to their regular assigned teams at 5 PM. They will observe the signout process of their team to the night float cross cover resident.
- After observing signout, the students can assist their team with any patient issues that are of educational value, study, etc., until 7 PM.
- At 7 PM, the students will report to Medicine Team C workroom (4th floor corner room near elevators) and pair up with a night float admitting resident. Students and residents should exchange contact information and ensure new admissions are communicated.
- As patients are admitted, students are expected to assess patients independently. Example:
- Patient 1 assigned to team A, student 1 on team A assesses patient
- Patient 2 assigned to team B, student 1 on team B assesses patient
- Patient 3 assigned to team C, student 2 on team A assesses patient
- Patient 4 assigned to team D, student 2 on team B assesses patient
- Students are excused from the call shift after completion of their admission.
- Sunday night shift admissions
- The decision on which student gets to admit the patient which stays on their team should be decided amongst the students (e.g., which student is student 1 on team A vs student 2 is decided amongst themselves).
- If you admitted patient 3 or 4 (and thus the patient did not remain on your team Monday morning), we recommend you follow-up on the patient’s outcomes, such as by reviewing the chart or talking with the other team’s residents and attending.
- Students should work with the night float admitting resident for basic communication to ensure that the student is given adequate information to identify the patient and his or her complaint, sign-out from the ER, etc. Furthermore, the student should share any concerns about the case with the resident to ensure quality patient care. However, the night float resident is NOT expected to teach the student, such as review the assessment/plan. As with other admissions, however, the student is expected to review the case with the daytime senior resident on Monday morning in order to be prepared for attending rounds.
- Because the team C workroom can get crowded and students are familiar with their regular workspace, students can work in their regular assigned team rooms during the shift.
- MS4 subinterns will follow same schedules and duty hour restrictions as PGY1 interns
Didactics
- MS3s should be excused for required didactic sessions, including clinical vignettes, reflections, physical exam rounds, etc.
- Reminders of required sessions will be sent out by clerkship coordinator
Evaluations
- Senior residents will receive electronic evaluations for medical students through New Innovations. Please complete this in a timely manner (as this may delay final grading)
- Only senior residnets or (preferably) attendings may complete structured observations of history taking and physicals for medical students
F. Professionalism
- You cannot refuse the admission when called by the ED. If you feel that accepting the admission would jeopardize patient care or keep you in the hospital past the duty hour limits, contact your attending.
- To avoid overwhelming the night float residents, if you are called for a late admission and feel that you can admit this patient without violating duty hours, please do so
- Do not argue with the emergency department, other services, or your colleagues. Any issues should be brought to the attention of your attending or a chief resident.
- If you ever feel like you are overwhelmed, ask your chief resident and/or attending for help. We are here for you.
- Please respond to your pages in a timely manner, ideally within 15 minutes.
- You are accountable for checking your emails at a minimum of every 24 hours.
- On days off or when leaving the hospital, please leave an out of office message on your pager with the appropriate contact information of the covering physician. If any pages accidentally come through -- please try to provide callers with the appropriate person to call.
G. Anonymous Feedback If you have concerns you would like to report anonymously, please go to resident website (www.medicine.uci.edu/residency). Home page > Resident Resources (left menu) > Anonymous Feedback (top left) Please complete the form, providing as much detail as possible. If you would like a personal response, you may either provide your actual name or an outside, non-UCI email address (to main anonymity). Additionally, all responses will be included in weekly Friday Follies emails.
|
|



